Importance of Hormones - Female
It is useful to look at the natural process – a woman’s ovulatory cycle and the production of sperm in the male – and the hormones that play a major role in those processes – to help you to understand the causes of infertility, the role of modern infertility treatment in assisting conception,
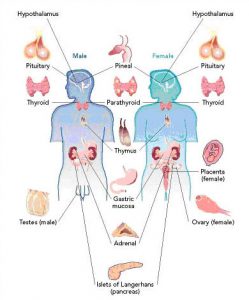
The gonadotropins (FSH and LH) are hormones that primarily affect the ovaries and the testes. They regulate the development and hormone-secreting functions of these organs and contribute to the production of sperm in the male and to the development and maturation of eggs (oocytes) in the female. Three gonadotropins are essential to reproduction: human follicle stimulating hormone (hFSH), human luteinizing hormone (hLH) and human chorionic gonadotropin (hCG). FSH and LH are secreted by the pituitary gland situated beneath the brain (see illustration 1). Their secretion is controlled by another hormone, the gonadotropin-releasing hormone (GnRH) produced by the hypothalamus. hCG is primarily produced by the placenta following successful implantation, and plays a role in maintaining pregnancy
The success rates in ICSI are greatly influenced by the quality of sperm preparation and by the skill of micromanipulation. ICSI, combined with IVF, is the most effective treatment for male infertility with a success rate of 20-25% of treatments resulting in a live birth.
Female Hormones
The main feature of a woman’s reproductive years is the menstrual cycle. This process, in which an egg (oocyte) ripens and is liberated every month ready for fertilization, is controlled by an elaborate system involving the gonadotropins hormones.
A women’s monthly menstrual cycle occurs in three phases:
- Follicular phase: Days 1 to 13.
- Ovulatory phase: Around day 14.
- Luteal phase: Days 15 to 28.
The cycle is controlled by the following hormones:
- Follicle stimulating hormone (FSH)
- Luteinizing hormone (LH)
- Oestrogen
- Progesterone
Day one of the menstrual cycle is marked by the first day of the menstrual bleeds. The first phase of the cycle is called the follicular phase and lasts approximately 14 days. The second phase, after ovulation, is called the luteal phase (1).
The number of eggs that a woman can produce in her lifetime is determined before birth. During her embryonic life, millions of special germ cells are produced in the ovaries. Many of them degenerate and the rest are ready to develop into mature eggs when the time comes.
Three months before ovulation, up to 300 eggs are recruited for growth and development. Each of the eggs is contained in a fluid-filled sac or ‘follicle’ that surrounds and nurtures it during development (5). About two weeks before ovulation, the secretion of FSH rises (3), stimulating the growth and development of the follicles. The growing follicles secrete increasing amounts of the hormone oestrogen (4), which causes the lining of the uterus (or endometrium) to thicken (6), and promotes changes in the cervical mucus that enable optimal penetration of the sperm.
Under the influence of FSH, one ‘dominant’ follicle grows and matures faster than the others that then degenerate (5). About 32 hours before ovulation, oestrogen secretion peaks, causing a surge in the production of LH (3,4). This triggers the release of the mature egg from the dominant follicle (5). What remains of the follicle is subsequently transformed into the corpus luteum, which secretes progesterone to prepare the endometrium for implantation (5). Due to the progesterone, the body temperature rises (2).
If the egg is not fertilized by a sperm within 72 hours of its release from the follicle, the corpus luteum will ultimately degenerate and menstruation occurs (5). However, if fertilization does take place and the resulting embryo continues its development, hCG is produced. This causes the corpus luteum to secrete the two hormones oestrogen and progesterone to ensure favourable conditions for the implantation of the fertilized egg. In fact, the presence of hCG in the serum or urine is the first indicator of early pregnancy.